What is the Connection Between Mental Health and Migraine, and How Can This Lead to Burnout in the Workplace?
Mental health disorders, migraine, and their connections
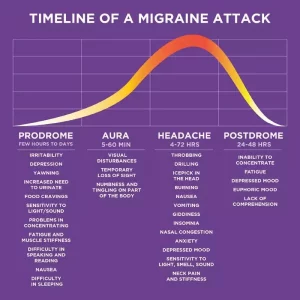
A mental health disorder, or mental illness, is a medical condition and affects a person’s mood, thinking, or behavior. 1 Common examples include anxiety, depression, and bipolar disorder. Migraine is a neurological disease and a primary headache disorder with symptoms such as headache, nausea, and sensitivity to light, sound, and smell. 2
Migraine is not a mental health disorder. Migraine is a complex neurological disease. However, the relationship between migraine and mental health is complex and likely bidirectional. 3
Migraine and mental health disorders often occur alongside one another.
Migraine and many mental health conditions are comorbid, meaning that they occur in a higher likelihood together than they occur in the general population.
There are both physiological and psychological reasons why migraine and mental illnesses occur together.
The full connection as to why these conditions frequently occur together is still not understood. According to Dawn Buse, an associate professor in the Department of Neurology at Albert Einstein College of Medicine and the director of Behavioral Medicine at the Montefiore Headache Center, “We think there might be some underlying reason, maybe a genetic reason, or the fact that both depression and migraine act off similar biochemicals in the brain and in the body that predisposes someone to have one, and then the second.” 4
Living in chronic yet unpredictable pain takes an emotional toll.
Along with the physiological connections, there is also a strong emotional component of how living with an unpredictable and disabling chronic health condition can affect your life. Chronic pain (like migraine) and mental health can mutually exacerbate each other, leading to additional physical and psychological complications. 5 People with migraine are forced to miss out on social events, job opportunities and promotions, and special occasions. This leads to social isolation, which can exacerbate mental health conditions. 6 In light of the chronic pain and poor treatment that many people living with migraine experience. It is perhaps not surprising to see higher levels of depression and anxiety among this population.
Cephalalgiaphobia refers to the cycle of fear and anxiety created by unpredictable or frequent migraine attacks.
The term cephalalgiaphobia translates to ‘fear of head pain’ and describes the anxiety of never knowing when the next migraine attack may strike. 7 Stress can trigger a migraine attack, and a migraine attack often causes additional stress. 8 People who experience regular attacks may become trapped in a vicious cycle of worrying whether they will be able to attend an event, or complete an assignment, and this stress alone can then trigger or exacerbate the next migraine attack.
Mental illness can increase the frequency of migraine attacks.
Untreated mental health conditions can exacerbate migraine and is a risk factor of chronification. Migraine becomes chronic once an individual experiences at least 15 headache days per month, 8 of which have additional migraine symptoms. 9
Migraine has connections with many mental illnesses:
Depression
People with migraine are 2.5 x more likely to experience depression. One study found that in patients with migraine, 41-47% of them also had depression. 10
Anxiety
People with migraine are 2-5 x more likely to experience an anxiety disorder than the general population, and more than half of those with migraine will experience an anxiety disorder throughout their lifetime. 11 The most common anxiety disorders in those with migraine are generalized anxiety disorder, panic disorder, and obsessive compulsive disorder. 12
Post-Traumatic Stress Disorder
Also an anxiety disorder, post-traumatic stress disorder (PTSD) is also more common in those with migraine. Those with episodic migraine are 3-4 x more likely to also experience PTSD. 13 Those living with both migraine and PTSD are more likely to lose more work days and experience greater disability compared to those with migraine and no PTSD. 14 Interestingly, both migraine and PTSD are 3x more likely in females than males. 15
Bipolar Disorder
People with migraine with aura are about 3 x more likely to also have bipolar disorder. In addition, of those living with bipolar disorder, about 1/3 also have migraine disease. 16 Those with comorbid migraine may have a higher risk of an unstable rapid cycling course of their bipolar disorder. 17
Suicide
Those with migraine have 3 x the rates of suicide than the general population. 18 The chances of suicidal ideation, suicide plans, and suicide attempts increase in those with migraine. 19
(If you are experiencing suicidal thoughts, please reach out to your doctors, loved ones, or the Suidide Hotline at 1-800-SUICIDE , 1-800-784-2433.)
Other Psychiatric Conditions
Migraine is more common in those who have suffered from abuse, whether the abuse was emotional, sexual, physical, or neglect. 20 Those with migraine are more likely to live with attention deficit hyperactivity disorder (ADHD). 21 In addition, there are many other psychological comorbidities of migraine.
The impact of mental health in the workplace
Mental health can affect multiple aspects of a person’s life, including their work life. Many would argue that employers hold an obligation to ensure that their employees have the opportunity to access resources to help address both mental and physical health issues.
Nearly 1 in 5 Americans live with at least one mental health disorder. 22 Americans are one of the most stressed populations worldwide, with 55% of Americans experiencing daily stress- 20% above the global average of 35%. 23
Stress is costing US employers billions.
This stress isn’t something employees can just leave at the door. 83% of US workers suffer from work-related stress. Stress causes 1 million Americans to miss work each day, and costs US businesses $300 billion each year. 24 The National Safety Council estimates that companies spend $15,000 a year on each employee experiencing mental health issues. 25 The CDC reports that depression alone has an annual toll of 200 million lost workdays to American businesses. 26 In addition to this, migraine is also costing employers billions of dollars annually.
Stigma of both migraine and mental health disorders prevent employees from seeking help.
Stigma prevents people from disclosing these conditions and requesting support. Less than 30% of employees feel comfortable disclosing a mental illness to their employer, and less than 25% feel comfortable notifying human resources. 27 The stigma of migraine also prevents employees from seeking assistance at work.
Effective workplace programs for both migraine and mental health exist.
Fortunately, there are effective management strategies for both mental health disorders and migraine in the workplace. For mental health, strategies such as Employee Assistance Programs, with free and anonymous mental health assessments and treatment options, and comprehensive health insurance plans can benefit employees. More detail about these and other strategies are discussed at the end of this article.
As for migraine, there are numerous studies- including those covered in the Harvard Business Review– which highlight effective workplace programs. 28 Simple education programs, such as newsletters, webinars, or lunch conferences, can help employees identify both the diagnosis and treatment options for migraine. A literature review of multiple studies proves that these programs can increase productivity by 29-36%. 29 Accommodations for migraine in the workplace have proven effective and inexpensive. These programs can drastically reduce the cost of migraine for both employee and employer. As migraine improves, improvements in depression and anxiety may also occur, creating a virtuous cycle. Contact us today for a free survey to determine the prevalence of migraine in your office.
If mental health disorders, migraine, and / or other health issues continue to go unaddressed, deteriorating health and burnout amongst employees may occur.
What is employee burnout, and how can it be prevented?
According to Forbes, workplace burnout is the “extreme physical and emotional exhaustion that results in a lack of professional efficacy, increased cynicism, lack of engagement and depleted energy.” 30
Burnout worsens employee medical conditions.
Burnout leaves employees at risk of worsening current medical conditions like migraine and mental health disorders, and potentially triggering new medical conditions such as high blood pressure, insomnia, substance abuse, heart disease, and vulnerability to contagious illnesses. 31
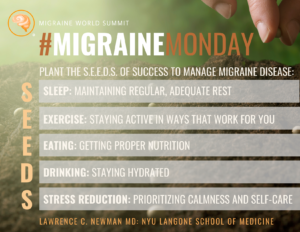
Taking steps to prioritize health and prevent burnout in your office may be easier than you think.
Consider the following measures to prioritize mental wellness in your office.
– Strive to create a supportive company culture where employees do not feel stigmatized and afraid to disclose any medical conditions such as migraine or mental illnesses. Getting support as soon as possible can help prevent burnout. Implement mandatory manager trainings on how to address mental health and migraine in the workplace.
– Lead by example. Employees seeing their managers embrace support options for mental health can pave the way for these employees to feel supported in accepting these resources. 32
– Offer accommodations like flexible scheduling and remote working.
– Offer an Employee Assistance Program, providing mental health assessments and counseling services for a variety of stress coping mechanisms and mental health services. 33
– Consider policies such as unlimited paid time off (PTO), so that employees are not intimidated to take advantage of mental health days. 34
– Provide comprehensive health insurance plans which will enable your employees to address these conditions before they are forced to exit the workplace. 35
– Make meaningful changes to help reduce stress in the workplace. Take preventative measures to help root out the actual causes of workplace stress like high job strain, a lack of social support, poor management, and poor recognition and compensation, instead of simply trying to ease the symptoms of workplace stress and burnout. 36
– To learn more about how specific companies have implemented successful mental health programs in the workplace, visit the CDC’s website here. 37
Whether it’s for migraine, a mental health disorder, or any other type of illness or disability, by not providing employees with proper support, the company is paying for it in lost productivity, lower retention and staff satisfaction. These losses accrue to the bottom line in each business. They also play a role in the employer’s ability to attract and retain top talent. Reach out to us today for free or paid services to better support your employees with migraine or mental health issues.
1)Mayo Clinic Staff, 2019, Mental Illness, Mayo Clinic, <https://www.mayoclinic.org/diseases-conditions/mental-illness/symptoms-causes/syc-20374968>
2)2021, Migraine headaches, Cleveland Clinic, <https://my.clevelandclinic.org/health/diseases/5005-migraine-headaches>
3)Breslau, et al, 2000, Headache and major depression: is the association specific to migraine?, Neurology, <https://pubmed.ncbi.nlm.nih.gov/10668688/>
4)2018, Understanding the relationship between migraine and mental health, American Migraine Foundation, <https://americanmigrainefoundation.org/resource-library/link-between-migraine-depression-anxiety/>
5)IsHak, et al, 2018, Pain and Depression: A Systematic Review, Harvard Review of Psychiatry<https://pubmed.ncbi.nlm.nih.gov/30407234/>
6)Novotney, A., 2020, The risks of social isolation, American Psychological Association, Monitor on Psychology, <http://www.apa.org/monitor/2019/05/ce-corner-isolation>
7)Giannini, et al, 2013, Cephalalgiaphobia as a feature of high-frequency migraine: a pilot study, Journal of Headache and Pain, <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3686604/>
8)2017, Stress and Migraine, American Migraine Foundation, <https://americanmigrainefoundation.org/resource-library/stress-migraine/>
9)Minen MT, Begasse De Dhaem O, Kroon Van Diest A, et al, 2016, Migraine and its psychiatric comorbidities, Journal of Neurology, Neurosurgery & Psychiatry, <https://jnnp.bmj.com/content/87/7/741>
10)Minen MT, Begasse De Dhaem O, Kroon Van Diest A, et al, 2016, Migraine and its psychiatric comorbidities, Journal of Neurology, Neurosurgery & Psychiatry, <https://jnnp.bmj.com/content/87/7/741>
11)Minen MT, Begasse De Dhaem O, Kroon Van Diest A, et al, 2016, Migraine and its psychiatric comorbidities, Journal of Neurology, Neurosurgery & Psychiatry, <https://jnnp.bmj.com/content/87/7/741>
12)Baskin, et al, 2006, Mood and anxiety disorders in chronic headache, Headache, <https://pubmed.ncbi.nlm.nih.gov/17034402/>
13)Peterlin, et al, 2014, Post-Traumatic Stress Disorder and Migraine: Epidemiology, Sex Differences, and Potential Mechanisms, Headache, <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3974501/>
14)Rao AS, Scher AI, Vieira RV, et al, 2015, The impact of post-traumatic stress disorder on the burden of migraine: results from the national comorbidity survey-replication, Headache, <doi:10.1111/head.12698>
15)Peterlin, et al, 2014, Post-Traumatic Stress Disorder and Migraine: Epidemiology, Sex Differences, and Potential Mechanisms, Headache, <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3974501/>
16)Fornaro & Stubbs, 2015, A meta-analysis investigating the prevalence and moderators of migraines among people with bipolar disorder, Journal of Affective Disorders, <https://pubmed.ncbi.nlm.nih.gov/25801521/>; Minen MT, Begasse De Dhaem O, Kroon Van Diest A, et al, 2016, Migraine and its psychiatric comorbidities, Journal of Neurology, Neurosurgery & Psychiatry, <https://jnnp.bmj.com/content/87/7/741>
17)Gordon-Smith K, et al, 2015, Rapid cycling as a feature of bipolar disorder and comorbid migraine. J Affect Disord;175:320–4. <doi:10.1016/j.jad.2015.01.024>
18)Fuller-Thomson E, Hodgins GA. Suicide attempts among those with migraine: findings from a nationally representative Canadian study. Arch Suicide Res. (2019) 24(Suppl. 1):360–79. doi: 10.1080/13811118.2019.1578710, <https://www.tandfonline.com/doi/abs/10.1080/13811118.2019.1578710?journalCode=usui20>
19)Minen MT, Begasse De Dhaem O, Kroon Van Diest A, et al, 2016, Migraine and its psychiatric comorbidities, Journal of Neurology, Neurosurgery & Psychiatry, <https://jnnp.bmj.com/content/87/7/741>; Berhane HY, Jamerson-Dowlen B, Friedman LE, Berhane Y. Association between migraine and suicidal behaviour among Ethiopian adults. BMC Psychiatry. (2018) 18:46. doi: 10.1186/s12888-018-1629-7
20)Gretchen E Tietjen & B Lee Peterlin, 2011, Childhood abuse and migraine: epidemiology, sex differences, and potential mechanisms, Headache, <https://pubmed.ncbi.nlm.nih.gov/21631473/>
21)Fasmer, et al, 2011, Adult attention deficit hyperactivity disorder is associated with migraine headaches, European Archives of Psychiatry and Clinical Neuroscience,<https://pubmed.ncbi.nlm.nih.gov/21394551/>
22)2019, Mental Health in the Workplace Mental Health Disorders and Stress Affect Working-Age Americans, Center of Disease Control and Prevention, https://www.cdc.gov/workplacehealthpromotion/tools-resources/workplace-health/mental-health/index.html>
23)2019, 42 Worrying Workplace Stress Statistics, The American Institute of Stress, <https://www.stress.org/42-worrying-workplace-stress-statistics>
24)2019, 42 Worrying Workplace Stress Statistics, The American Institute of Stress, <https://www.stress.org/42-worrying-workplace-stress-statistics>
25)2021, ≥, NSC and NORC at University of Chicago, <https://www.nsc.org/newsroom/new-mental-health-cost-calculator-demonstrates-why>
26)Minor, 2021, Mental Health In The Workplace: The High Cost Of Depression, Forbes, https://www.forbes.com/sites/mariaminor/2021/01/20/mental-health-in-the-workplace-the-high-cost-of-depression/?sh=dcfb956666ff
27)Bertsos, 2020, The New Rules of Taking a Mental Health Day From Work, Thrive Global, <https://thriveglobal.com/stories/the-new-rules-of-taking-a-mental-health-day-from-work/>; 2019, Mental Health at Work, Mind Share Partners, <https://www.mindsharepartners.org/mentalhealthatworkreport>
28)Begasse de Dhaem, 2021, Migraines Are a Serious Problem. Employers Can Help, Harvard Business Review, <https://hbr.org/2021/02/migraines-are-a-serious-problem-employers-can-help>
29)Begasse de Dhaem, et al, 2020, Identification of work accommodations and interventions associated with work productivity in adults with migraine: A scoping review, Cephalalgia, <https://pubmed.ncbi.nlm.nih.gov/33302697/>
30)Kurter, 2021, Employers, Here Are 4 Ways You Can Begin To Effectively Tackle Employee Burnout, Forbes, <https://www.forbes.com/sites/heidilynnekurter/2021/04/27/employers-here-are-4-ways-you-can-begin-to-effectively-tackle-employee-burnout/?sh=57c9af316009>
31)Mayo Clinic Staff, 2021, Job burnout: How to spot it and take action, Mayo Clinic, <https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/burnout/art-20046642>
32)Bertsos, 2020, The New Rules of Taking a Mental Health Day From Work, Thrive Global, <https://thriveglobal.com/stories/the-new-rules-of-taking-a-mental-health-day-from-work/>
33)What is an Employee Assistance Program (EAP)?, U.S. OFFICE OF PERSONNEL MANAGEMENT
,<https://www.opm.gov/faqs/QA.aspx?fid=4313c618-a96e-4c8e-b078-1f76912a10d9&pid=2c2b1e5b-6ff1-4940-b478-34039a1e1174>
34)Sammer, 2020, 4 Lessons About Unlimited Vacation, Early adopters share what they’ve learned so far, SHRM, <https://www.shrm.org/resourcesandtools/hr-topics/benefits/pages/4-lessons-about-unlimited-vacation.aspx>
35)2021, Cost Effectiveness Infographic, Headache and Migraine Policy Forum, <https://static1.squarespace.com/static/5886319ba5790a66cf05d235/t/61a66c28d397313ed8ce809f/1638296617697/HMPF_CostEffectiveness_Infographic_Dec2021.pdf>
36)Stansfeld, et al, 2006, Psychosocial work environment and mental health- a meta-analytic review, Scandinavian Journal of Work, Environment & Health, <https://www.jstor.org/stable/40967597?seq=1#page_scan_tab_contents>
37)2019, Mental Health in the Workplace Mental Health Disorders and Stress Affect Working-Age Americans, Center of Disease Control and Prevention, https://www.cdc.gov/workplacehealthpromotion/tools-resources/workplace-health/mental-health/index.html>